Podcast
December 10, 2025
From NHL Cardiologist to Health Tech Innovator, with Dr. Gregory Sanders

In this episode of The Innovators, Dr. Greg Sanders, a practicing cardiologist and the Founder & CEO of Hybrid Chart, takes us through his path from clinical practice to launching a healthtech company. He discusses the challenges faced in the healthcare industry, including rising costs, administrative burdens, and the resistance to change among medical professionals. Dr. Sanders emphasizes the importance of teamwork and support in both medicine and entrepreneurship, and offers valuable advice for healthcare leaders looking to improve processes and patient care through technology.
Kaled Alhanafi (00:00.16)
Welcome to the innovators podcast. I'm your host Khalid Al-Hanafi, CEO, co-founder of Basara. And today I am so excited to welcome to the podcast, Dr. Greg Sanders, cardiologist, but also started a company, a startup and wrote the initial code for it. So I am really excited to talk to you when we're talking about innovation and healthcare. Thank you and welcome to
Thank you for having me.
Kaled Alhanafi (00:31.8)
We'd love to start with just learning more about yourself. How did you start as a cardiologist? And then maybe we can talk a little bit about your journey later on into the startup world.
Dr. Gregory Sanders (01:08.61)
So I have an unusual story because it started when I was 14 years old, back in the 1800s when I got a computer. There weren't a lot of them back then, it was an Apple IIe. And so I started as a developer, I started as a coder. I taught myself assembly language on an Apple IIe. I started a software company sort of when I was 16 before cardiology. I was 14 by accident where I was writing code for businesses. then I got into medicine. at that time in that age, the thought of me being a software developer or owning a software company didn't even seem like a real job. So I went into medicine. somewhere in, I think I was a third year medical student and I was sitting, I standing in the OR like holding a retractor and some nurse came in and said, someone's on the phone because something's crashed. And I was like, I can't do both. So I sold that whole little project off. Throughout my medical career, which led me through Boston and eventually to Arizona, I always have these sort of process improvement goggles on, where I'm always looking at different processes saying, I can fix this. And so using my skills as a not just software design, but it's also database design, the whole platform design, it's not just writing some code. And mirroring that with my unique perspective on what's actually happening in medicine, that that duality is what led me to develop hybrid chart. So I joined a group of excellent cardiologists in Phoenix as my first job, you know, and, and I started rounding and I realized like this whole thing is broken. Like in the office we were fine, but the second I got out into the world where there were all these hospitals and we had to report back what we were doing and charge for it and all that, the whole thing was completely broken. And so I took it on myself to solve that problem for my own practice, which then sort of bubbled into.
Kaled Alhanafi
So you started at, you started writing code first, then figured, that's not gonna be a career, I'm gonna go into medicine, chose cardiology, went and did that. And then because you already had this process-oriented nature, looking for challenges, problems, how to streamline them, you found in your practice some problems, and you started Hyperchart.
Dr. Gregory Sanders (03:16.718)
Yeah, and I sort of had this habit of writing code along the way. So at my residency program, our entire call schedule with the hospital operators ran on my software. At Harvard, where I did my fellowship, I was innovating and writing databases for echocardiography and search engines for doing research papers. So everywhere I went, I kind of left a little footprint of, hey, here's a cardiology coder who solved the problem.
The one I solved here was a tough one because it's a big it's a big process and luckily for me You know when I first started doing it there were no self there what there were cell phones, but they were flip phones You there were no smartphones. That's right every hospital didn't have Wi-Fi every hospital didn't have a computer terminal everywhere so we kind of grew up with the technology as it grew up and obviously now it's a different playing field but But we grew into that space. I think very nicely that's
Kaled Alhanafi
That's incredible. How did you, so you're a cardiologist, you see patients every day, that's what you do even today, to this day. How do you balance all of that with this incredible other side career that you were kind of building from scratch in building hybrid chart? Both writing the code, but also now, I'm assuming it's much bigger, of course you've got a team. That's a lot, that's amazing that you're doing this.
Dr. Gregory Sanders
Yep. So I mean, I got to give some kudos to a lot of people because this is not a one man show. first of all, doctors, think, are under the impression that they know everything. And so I'm here as a doctor, everybody to dispel the myth. We don't know everything. And the quicker a doctor realizes that they don't know everything, they can't do everything on their own, the better it works out. So I would say at the beginning of the whole process, I leaned in heavily on my own practice to help me work out
some of the workflows and they get a lot of credit for helping me kind of smooth out some of the rough edges around it. Our first customers were local and they were cardiologists, gastroenterologists, cardiac surgeons here in town, people that I worked with or indirectly worked with. So, you know, there were people like Kevin Brady and Ken Ashton who were cardiac surgeons, who still are cardiac surgeons, who really helped me kind of mold this.
Dr. Gregory Sanders (05:39.778)
My own practice, Arizona Cardiology at the time, again, same thing, Cardiac Solutions, a local cardiology group in town were instrumental in helping me craft some of the, not just the workflows, but some of the innovation around how does a practice guide their own journey? How does a practice create something that's not hard-coded that is soft-coded to their specific needs? And we'll get into that later because that's...
kind of one of the secret answers to how do you fix healthcare. So I think in developing the software, launching the software, I needed help and I got help. The second it becomes a real company, and now we're in every state, we are definitely grown up, or don't think we're even considered a startup anymore. So now my big challenge is I need help.
on the cardiology side. So I need a team of people that I can lean on who are there for me, who support what I'm doing. And I need a team on the hybrid chart side, which I have, who I can lean on, who I trust to run the business, who I trust to, you know, work with me, innovate with me, because there's always constant process improvement as well. So I think the answer is I need teams of people on both ends, cardiology and software.
who I can rely on and who support what I'm doing. Not everybody supports this, right? So some people look at a physician innovator and go, pick one. Why? Why do I have to
Right. Yes. yeah, tell us why why not pick one because we talked about this and I think it's brilliant that you're bringing the two together, but maybe share with the audience why actually not pick one.
Dr. Gregory Sanders (07:25.058)
Well, I think the instinct everyone has is you're going to be more effective if you're more focused and you're not diluted. I think that makes sense. However, I'm infinitely more beneficial to my software development living and breathing the space I'm in every day. I'm infinitely more helpful as a cardiologist solving problems in my own practice based on the experiences I've
had and all the skills I've learned creating a software company and running a software company. So, you know, because you sort of become a project manager and you become you have a different eye for things. And even in my own practice, like I can craft better processes simply because I'm used to crafting better processes. So I I would argue if you have the right temperament for it, if you don't like sleep, if you enjoy crying in the shower every morning.
then I think this is for you, you know, and you should do it. But you need, but you need help.
That's great advice. Yes, you have to have a team on both sides. Tell us about your teams. How big are they today? Because you're leading the hybrid chart organization. as a cardiologist, you said you have a team around you. Tell us more a little bit about teams.
Dr. Gregory Sanders (08:47.714)
So we're lean and mean. mean, we're probably 17 or so on the hybrid chart side, spanning everything from development, biz dev, sales, marketing, implementation, support, account management. Everyone just thinks you just flip the thing on and here you are. Well, no, there's as you know, there's way more to it than that. And the irony of it is so we have our tool and it
solves a lot of different problems. There's a desktop, there's mobile app, and there's different personas using it. But if you look at our internal tool to manage the product, it is bigger than the product. Wow. Because you need to be able to troubleshoot, fix problems, monitor things, invoicing. So our internal tool is probably bigger than our actual tool. And that's what everyone forgets. You're going to need to maintain things. Yeah.
In your line of work, whether it's being a cardiologist or working on a chart, they're both in healthcare. And we talk to lot of CEOs, cardiologists, urologists, all these specialties. And what we see is they're being squeezed on both sides, right? As we know, costs go up, complexity goes up, they're trying to keep the team motivated, it's high-churn roles for lot of the admin roles, you're trying to keep...
Everything put together and then revenue is not necessarily keeping up. It's really hard to keep growing your revenue as well So what's your advice because you seem to have it balanced in a way where we've got really supportive teams the administrative side You've kind of figured out whether on the cardiology side or what the work that you do at hybrid chart to help others What's your advice to a CEO? Cardiologist someone in health care that is dealing with this pressure constantly
Well, you're bringing up some interesting points, which if we don't if you don't mind backing up a few pieces, of course. So if you look at health care, private practice, world health care in general over the last 20 years, right, the cost of doing business has steadily increased. Yes, like the cost of doing any business has increased salaries, rents, materials, da da da. Physician compensation has either gone down or been flat. So the margins
Dr. Gregory Sanders (11:14.04)
have been squeezed. So everyone else, every other sector, reimbursement goes up or top line revenue goes up, cost of doing business goes up, you maintain your margin, you figure out ways to increase your margin. There's been a steady decline or a flat line of physician compensation that's been frozen for more than 20 years. And then they bundle things together. They say, well, we used to pay you three bills for this, we're going to bundle it into two. And then when you do the math, you're like, wait,
That just went down. So at some point there's gonna be a line where the cost of doing business crosses the line of top line revenue and your margin is now zero or negative and now everyone's in big trouble. So that's a global problem which I don't think I can fix. I'm definitely not qualified to fix that. That is a problem that has driven a lot of doctors out of being an entrepreneur and back into I'm just gonna join a hospital system. The problem with that and.
Sorry, everyone out there who's working for a hospital, but productivity goes way down when you're employed. Quality of care goes down, sorry, when you're employed. Cost of care goes up when you're employed. So there's a huge incentive to keep doctors independent, keep doctors entrepreneurial, better care of patients, more efficient care of patients, cheaper care of patients. So that's one global problem. At the same time, you got these doctors running around
who their time dedicated to actual patient care is shrinking, shrinking, shrinking. The current estimates are about 30%. Of a time spent by a doctor is actually taking care of a patient, 70 % is clerical work or other. Let's just put in the other category. Well, that's terrible. Administrative, driving to a hospital, whatever it may be. You're not doing medical decision, you're not having a doctor patient relationship, that's 30 % of it administrative.
Kaled Alhanafi (13:02.702)
I'm not taking care of patients.
Dr. Gregory Sanders (13:10.09)
So that's bad. And then on top of that, the demands that we're now asking the doctors to do to drive processes like population health management, quality of care outcomes, dare I say it, value-based care, right? Because everyone wants to move to value-based care. OK, well, how's that going to work? And we can talk about that, because I think hybrid chart does solve that, at least parts of it. So now we take these doctors who are stretched.
They're spending 30 % of the time doing the thing they were actually trained to do. The rest of it is all clerical stuff. And then we keep piling more stuff on top of them. Like now you got to do this. Now you got to push this button. Now you got to check that box. Now you got to fill out this form because the patient has pneumonia. And now physicians are burning out. and by the way, while we're doing all these demands, remember that margin keeps getting smaller and smaller and smaller. And then the RCM teams, they're being tasked
with how do I get these claims out properly? How do I fight for denials? The rules keep changing. How do I even, you know, so they're under the squeeze also of trying to make the margins as healthy as they can be. So everybody's under a squeeze.
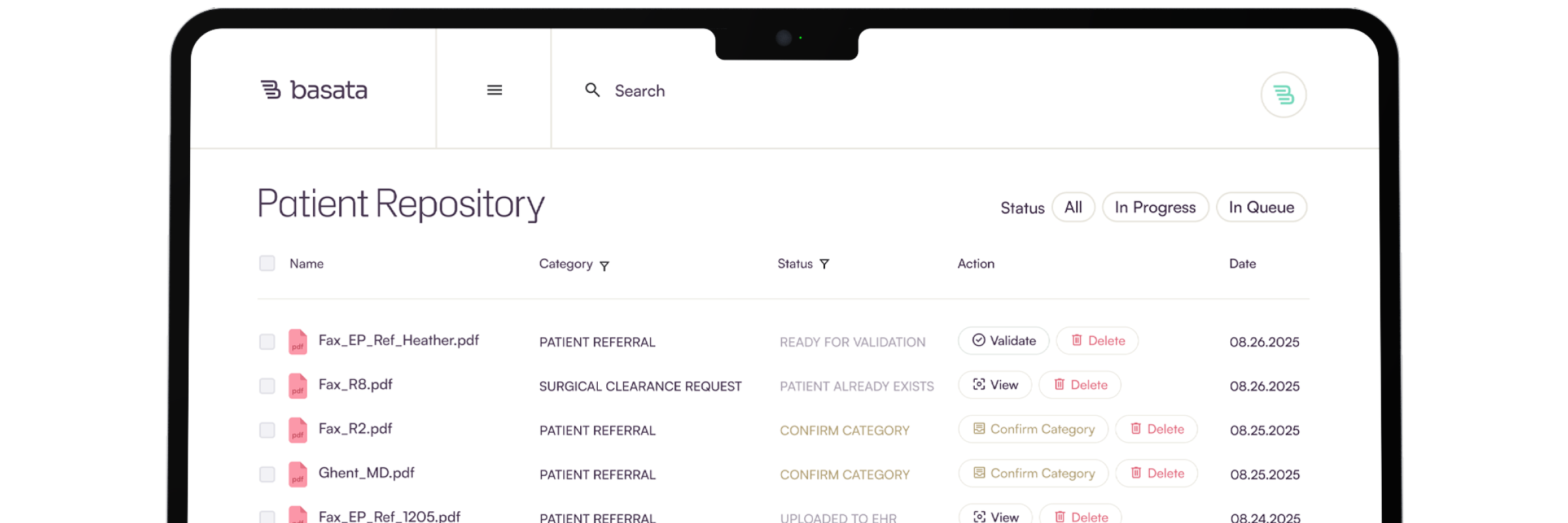
Yes, yes. Let's pause the conversation. Let me tell you about Basada. Basada is building the AI workforce for health care. We automate faxes, phone calls, and everything in between on the administrative side of health care so that you can focus on care. Less chaos, more care. To learn more, visit our website, basada.ai. Now let's dive back into the conversation. We say this often that if you go to any other industry, aside from health care, you take Amazon as a company, for example, right?
Your costs go up. Sure, with every company as you said, you simply move that and put it on the customer, the consumer, right? We all want boxes to come home. We, you know, it's around Halloween right now. We're all excited for that, right? We're getting these boxes and we're going to pay more for it. It's okay. We'll pay. In healthcare, unlike any other industry as you indicated, you can't really do that. You've got to schedule Medicare. You've got to stick to what you can charge. So your revenue...
Kaled Alhanafi (15:25.742)
is regulated, but your costs, of course, are not regulated. So that can balloon and the complexity as well. So talk about the churn, talk about all these problems. We were talking with another CEO of a practice and they shared with us that five of their call center people decided to go to lunch at McDonald's and never came back. They found jobs, 20 cents more, 25 cents more an hour. And they decided, I'm not going to come back for the call center and scheduling. I'm just going to do that. So not only are they squeezed, but it's also challenging operationally.
The staff turnover in healthcare is astounding. We are placing a lot of demands on people. And so when I say I have support, I think you probably assumed I meant the other doctors in my practice. No, no, no. I mean, I need nurses, my admin, my MAs, schedulers to be supportive of my endeavors because they have to make my schedule creative. They have to talk to patients. It's really the whole team.
And we do put a lot of demands on staff who some of them are, they don't have a master's degree in healthcare administration and they're doing the best they can. And it takes time to find the right culture, the right group. I've always had this struggle. I'm only as good as a doctor as my worst employee who answers the phone. Because, and sometimes I used to do this, I haven't done it in a while.
I love this.
Dr. Gregory Sanders (16:57.054)
I used to call my own office and just say, hey, I need to make an appointment. Just to kind of do the quality assessment of how am I being represented out there. And I see patients all the time, they go, hey, I need a new primary care doctor. I'm like, why? That person's great. And they go, well, I really like the doctor, but their office, like they don't call me back or they were rude to me or they didn't squeeze me in when I needed to be squeezed in or I never heard from them about a test result.
It has nothing to do with the doctor. That's right. It's the staff around the doctor. It's the process around the doctor, which is really frustrating because I don't have a lot of control. That's right. When patients come in and they usually apologize, they go, I'm sorry, I need to vent. I go, OK, well, go ahead, vent. And so they launch into a whole diatribe about my staff and what happened. And then they apologize again. They're like, I'm really sorry. And I go, no, no, no. If you don't tell me, how on earth would I know?
Please tell us about this.
Dr. Gregory Sanders (17:54.646)
I have no opportunity to fix this unless you bring it to my attention. And I'm not going to get that person in trouble necessarily, but I got to fix it. But I don't even know what's a problem unless you tell me. So my patients at this stage know that I'm an easy person to approach where they're having a problem.
That's great that they can share it with you. You'll help fix it. Yeah, and you're proud of that. We see this often by the way, it's not you know in your group only as you know, this is across the board you go look at a one-star review and it's never about it's very rarely about the medicine. It's typically about exactly what you said, right? They you know, I love doctors so and so they start that way by the way apologetic because they know this is the person caring for me, right? I love doctors so and so but that the staff never get back to me or
I waited for 15 minutes on hold. That doesn't tell me that they care about me, Or they got the referral, it sat there for two weeks before I heard back from them. And it's like, I need to get going. I need my procedure.
And these are processes that are broken within the practice. And at the same time, practices, and this is the big theme we hit with hybrid chart, which is practices are resistant to change. I have a whole talk I give on why doctors won't change. And it's not even the things you think. I'll send you the slide deck. It's a funny slide deck. And I have some funny slides in there where I have faucets pouring directly into electrical outlets and talking about poor design and things like that.
You should share that with me. I'd love to see
Dr. Gregory Sanders (19:26.882)
The reason why doctors are resistant to change, everyone just assumes that they're stubborn and that they know it all. That's not really it. And so we had to crack this nut because we show up with hybrid chart. Most of the time we're doing a consultative sale. So they don't even know they have a problem. They kind of do. They can't articulate it. They can't define it. And so we're showing them where your processes are broken. But they're very resistant to changing the process. I don't remember all the slides off the top of my head.
But I will tell you that one problem is that they are comfortable with the rickety process they put together because they know where all the levers and knobs are. Even though they'll tell you it's awful. And it was inherited from the generation before them that says, here's how we do it. When we round, we fill out a piece of paper and we write, put a little sticker on there and check off the boxes of what we did. And we put it in a bucket. And then the biller types it into our.
They know it. It's a mess, they know it's their mess. know it's ridiculous.
But when you tell them to change, they know where all the cobwebs are. They know where all the levers are. And so their biggest fear is, I'm going to lose control of this process. So that's one. The second fear they have is they are not only do they just lose control of the process, but now there's going to be no one there to help them. Their experience up until now is an EHR or some other software comes in and says, look how great we are. Here you go. And then they go.
I have a problem and then they look around and no one's there to support. So not only are going to take away my levers, but you're going to disappear and now I'm on my own. Right? So they're worried about that. Yes. So these are some of the themes that doctors in the end would rather stick with a clunky process that they know that they at least have some visibility on versus trusting it to someone else. And doctors have been burned.
Dr. Gregory Sanders (21:22.35)
Right. Every time an EHR came out, I had high hopes. I was like, oh, this is going to be great. Right. Like, finally. And then I got it. And I was like, uh, can I talk to someone, please? Like, why am I clicking 18 times to fill one medicine? this person even, designed this, do they even know what I do for a living? back, circle back to when we unpack hybrid chart for a doctor, we can train them in 28 minutes. And usually halfway through that 28 minutes, they stop us. They go, I got this. Understand.
This is so intuitive. built this around, like whoever built this clearly knows what I do for a living and knows the nuances. The difference between software that a doctor will say is garbage versus saying is great is so subtle that even the developers who generated the one that they think is clunky are shocked. They're like, what are you talking about? It works great. The doctor's like, you don't know. You don't know our workflow. It's weird. They miss it.
Kaled Alhanafi (22:19.662)
Yes.
So part of my journey was I'm living these problems, I'm solving these problems, I'm straddling the fence between I'm a developer and I'm living it. So I can build something super user friendly that really mirrors the actual workflow. My dev cycles aren't delayed by me trying to explain to a group of people who are very well intended but have no idea about health care. The first three iterations are going to be like, no, wrong. So now it's delayed. So I just did it myself.
Right at the beginning. So my my dev cycles were fast, right? But then I have to implement this into a group of people my original practice when I built hybrid chart I presented it to them and they very confidently look at me in the eye and said no, thank you I was like what what but didn't you see didn't you see and they said we're fine Yeah, No, that's their initial impression is work. We're okay this
good.
Kaled Alhanafi (23:17.982)
Don't change anything. Don't just touch it. It's so messy, it's so on a handle, holding it by a thread. Don't touch it.
Don't touch it. Right. And then here's another hidden secret that most people outside of health care don't understand. Most doctors are literally running paycheck to paycheck. Not them personally. Yeah. But their practices are OK. So any disruption. Yeah. Any disruption in our if there's if you mess up their process, which they admit is garbage. But if you mess it up and now there's a two month delay in reimbursements coming in. They can't make payroll. That's right. Right. So they are and about the squeeze.
Dr. Gregory Sanders (23:55.084)
very very scared of changes to their RCM systems Right and along the way every time they roll out a new EHR It's so disruptive and it's and it's and and doctors are just moaning groaning complain and everybody moans
Yes.
Kaled Alhanafi (24:11.863)
I heard that on a sales call yesterday. The doctor there was like, we don't want click fatigue. We don't want click fatigue. And that was a term that was like, yeah, that makes sense. 18 clicks to get somewhere, that's a problem.
Awful. Took an interesting approach with hybrid chart and this was my own insertion of, I have a list of demands. Like if I'm gonna make a company, we're gonna do it my way. So when I first got my first EHR and I'm not gonna call out who they were, we rolled it out, 18 clicks to fill in a prescription was the least of the problems. And I walked into my office manager and I said, listen, I gotta talk to somebody over there. Like get me in front of some of these developers.
We need to fix a lot. And she laughed in my face. She was like, wait, you think you're going to get to talk to the dev team? Like, no. We put in a ticket three weeks ago. They still haven't called us back for a support ticket. You think you're going to talk to the dev team? Like, you're out of your mind. So when I started a hybrid chart, I said, all right, guys, first of all, we're a customer service company. So we are not waiting three weeks to call anybody back. We are calling everybody right away.
We are we are you get to know their dog's name you get to know their cousin's name you get to know your practices workflow in and out and we are a customer support That's right number two everybody who is a customer of hybrid chart once a year by default is invited to meet with our dev team We want to hear what do you like? What do you not like? What do you need? We have learned so much Now we don't charge for the development but the customer doesn't own that piece, right? So it's a community, this is a community approach. We're all gonna build a better tool together. And the biggest resistance to a doc, so let's say I did get in touch with my developer of that first EHR. And let's say they actually took the time to listen to me. I promise you, they would have said, yeah, we can do that for you, here's a bill for that development. So the barrier for making the tool better is,
Dr. Gregory Sanders (26:18.666)
A, they don't want to talk to me, and B, they're probably going to charge me.
So and then you're a practice that is being squeezed that doesn't have the margins to pay for anything strikes against you. So imagine if, so I wanted to remove those barriers, so I was like, okay, they get in front of us by default. And any good ideas they have that are applicable to everybody, that's not like only going to help them and them only. Let's dev it, let's dev it fast. So we're going to say, you're not going to see this in three years, you're going to see this in three months, because we do usually quarterly releases. You're going to get in three months. But then they just made the tool better.
So let's go back to me not knowing everything as a doctor. Even if I thought I understood the cardiology workflow, hybrid chart is good for every specialty. What do I know about being a urologist? Nothing. What do I know about being a nephrologist? Nothing. So I needed these practices through the open development model to help us create a better tool for their specific specialty so that it mirrored their world also. And if you don't do that, then they would say, well, this works really well for a cardiologist, but not so well for a gastroenterologist. and I didn't want to hire a gastroenterologist as a consultant because by the way, those physician consultants, they mean well, but they usually don't have an eye for what the product needs. And that's a big problem.
Kaled Alhanafi (27:47.843)
It's a huge problem. And back to the idea of advice to those folks that are listening, right? Maybe they are a cardiologist or a CEO and in that situation and worried about change, right? What would you tell them? How would you take that first step? Maybe it's a leap of faith that you have to take, I don't know. how would you get them to take part in this innovation?
So if you're a practice and you're thinking we need to do process improvement, we need to bring in AI, we need to clean up a certain process, and I will tell you that COVID helped. It helped.
COVID forced practices who didn't even want to pronounce the word telemedicine to adopt. That's right. They had no choice. That's right. And then once all of a sudden they saw a process improvement, they got a little excited. Yes. And they said, wait, what else can we fix? So it actually did break down some barriers, which was great. That's great. So your practice forcing function.
Kaled Alhanafi (28:46.922)
Aside from all the madness of COVID, course. Of course. Of course.
But but what some one of the few good things that's right, that's right, was it did knock down a few barriers and let doctors kind of really open their eyes to process improvement a little bit. Yep. So all right. I'm a taste they did. Yeah. And they saw it work. And so and the government was smart. They knocked down a lot of the barriers that they had for reimbursement. They you know, there was a law that you couldn't do telemedicine across state lines. Well, they turned that law off during covid said, go for it.
Yes, you know, so and then they made the reimbursement the same as for an in-person visit, right? Like kudos to them for actually stepping up and removing some of the barriers and that work job. It did work. So, OK, we go back to a practice you you think you want to make a change. It's a very, very scary world out there. There's a lot of products. There's a lot of names you've never heard. A lot of noise, a lot of feature lists, a lot of stuff. So my best advice is first of noise.
Dr. Gregory Sanders (29:48.482)
Pick your biggest problem. identify, if you can't articulate your biggest top three problems in your practice right now, we can't talk yet. Go back, think about it, whiteboard it, and then come back to me what it is. So a very focused problem that you wanna solve first. Because you can't boil the ocean, so let's just pick one problem. Then what you need to do is do a little bit of market research to figure out which companies slash products in my problem that I want to solve exist, but then ask some very important questions. Which of them align with my EHR? Because it may be a great product, but it doesn't interface with what I'm using in my office always the number one question, by the way, as we go to all these practices, does it integrate with the EMR? And of course we do typically, but yes, that's the number one question.
How mature is the company? But more importantly, how mature is the product? Could be a very, very well-known company, but they're still in pilot and they have five customers using this tool. So do I like the company? Do I like the product? Does the product have the features I'm looking for? And then here comes the hardest part, everybody, because they're doctors or they're healthcare. What is the ROI? What is the true cost? Two different things. Now, doctors are very good at dissecting what's my problem, which product has the features I'm looking for. They're not as good at calculating ROI.
Kaled Alhanafi (31:20.172)
the business side in general.
And remember, things that are expensive cost may have huge multiple ROI returns, in which case it's worth it. Because sometimes doctors see the price tag and they go, no, I'm not doing it. But wait, you didn't even do the math. Right. That, yeah, it is expensive. But guess what? You're going to make 5x off of that. So it is worth it. Right. Or it's not expensive. But when you run the ROI model, you realize, I have to see, you know, it's going to take me three years to break even on this. It's not worth it. Right.
So pick a very focused thing, do some market research, find the products out there that meet your needs feature-wise, then do an ROI analysis, do a cost analysis, figure out if it's even in your budget doable, and then try to ask the question, how easy or hard is this gonna be to implement in my practice the way it is? And the answer's always gonna be, it's gonna be hard. And so that's when you need an internal champion. This is kind of what we do for Hybrid Chart.
So if we show up to a 50 physician group and say, OK, you guys are all using hybrid chart. We'll roll it out in two weeks. Can we? Yes. Will we? Absolutely not. And that will fall flat on its face. We have to pick internal champions. Start with a pilot. You start with a focused group. You iron out all the wrinkles. You get them excited. You get them working it. They internally sell it. Everyone's looking over their shoulders saying, well, when do I get that? That looks cool. Start with that.
Dr. Gregory Sanders (32:51.218)
By the time the naysayers, because there's always naysayers, get it, the product's been smoothed over, the rollout's been refined, everybody's got some momentum going. I mean, that's how you have to do it. So it is an arduous process. It's annoying. You're going to have people pounding their fists on tables saying, I'm not doing this. And sometimes you can't move forward.
Yeah, yeah, but if you have the champion we found that that is he that works, right? Just for the sake of the audience really quickly What does hybrid chart do and benefit? does it benefit hospitals doctors the rounding and all?
when you're in your office and you're a bunch of doctors who generally our software doesn't solve your problem unless you deliver care outside the office. Yes. Also or exclusively. You're a hospitalist, you're only in the hospital, we can help you. Right. You're a bunch of doctors who have offices but you also go to hospitals, rehab centers, surgical centers, we can help you. Yes. Because the reality is when you're in your office you have a process built in. Your EHR has a schedule, your EHR has charts, you have people sitting right there to help you. The second you
walk out of the office into the wild, wild west, you have nothing. And when you leave doctors to piece together their own workflow, it's with scotch tape and dental floss. I mean, it's not good. It's bad. There's a lot of wasted time. There's a lot of communication that doesn't need to happen. There's a lot of stepping on each other's toes. There's handoffs between night call and weekend call. Who do I see at the hospital? There's consults coming in. There's people going home. It's a mess.
Absolute mess. Yes, and then when you're out there nobody in that hospital works for you So you're not putting in your charges in epic. Yeah at the hospital They don't work for you, right? You're writing it down and then you're bringing it back to the mothership and handing it to someone who has to key it in so hybrid chart solves Four major problems and I'm gonna start this conversation by telling you that this is not why I built high
Kaled Alhanafi (34:53.08)
Yes. Okay.
I had to build these four things to get the doctors to agree to use the tool. Once they were using the tool, then I'm going to tell you the part that I built for the real reason. Great. So the four things that we solve, almost like a ruse to get the doctor, because they can only see like one foot in front of their face anyway, we're going to solve your problems, Doc. We got you. So one is census management, which is coordinating where are my hospitals? Who do I need to see? Who's already been seen? Handoffs.
basically workforce allocation. Real time stuff. So we take somebody who's a practice who's clunky, they're immediately organized, they immediately get back at least an hour a week of time they were just.
just manning the hospital around, yeah.
Including staff at the office. Usually there's one or two people who are helping manage the whole inpatient workflow. Don't need those people anywhere. I mean, don't fire them. Just put them somewhere else. Number two, charge capture. So let's remove all the paper. Let's remove all the delays. If you look at the delay from when a doctor delivers service for when the claim goes out in the hospital, it could be a month. Just because the process is clunky. Or two seconds to do a charge capture.
Kaled Alhanafi (35:48.29)
Yes.
Dr. Gregory Sanders (36:07.63)
on a hybrid chart, we figured out for something complicated or easy, it's two seconds for the doctor, flows right into your EHR and off it goes. And there's a lot of intelligent logic built into our charge capture system where the RCM team's know-how is embedded in our software so they don't have to do as much coding on their end. So we grease the wheels on making sure all the charges go through and we also embed a lot of the RCM's intelligence on the front end.
Yes. Number three is internal communication, so secure communication. Doctors are notorious for texting each other stuff. You're not allowed to do that. Office staff are texting doctors in the field saying, hey, you have a new consult or call this nurse at this number about this patient. No, you can't do that. So it's census management, charge capture, secure communication, and then. or you're HIPAA Then the fourth one, everyone said, why on earth are you doing this? And I looked them in the eye and I said, this is the most.
Dr. Gregory Sanders (37:10.746)
Almost there. We're almost there. We're on number four. So four is discharge management. Patients coming off the list, patients going home. There's a huge chasm between inpatient world and outpatient world. How do you make a follow-up visit for this patient? How do you order testing for this patient? How do you flag them as a high-risk readmission patient? If I go to a practice that's not using hybrid chart and I go to their office staff and I say, who's in the hospital right now? They go, I have no idea. Who's being discharged today? No clue. So what happens is
A patient goes home. Three days later, they call the office. They wait on hold for 45 minutes. They finally get somebody if they don't hang up. They say, hey, I just got out of the hospital. And the staff are like, oh, wow, didn't know that part. And then they say, I need to see Dr. Sanders. They're like, he's busy. He's pretty busy. I don't know. You're going to get in. And so a lot of patient dissatisfaction, not good care. Staff are in the. They didn't even know that this person came out of the hospital.
Here's the classic story I tell and this is years ago. I'm in the hospital. I did my charge capture for two seconds. I Knew this patient was going home. So I tap tap tap on my phone. I got three taps. I already made their fall up I basically alerted my staff. They're coming out of the hospital. They're you need a fault when they need an echo they need lab testing. Right then and there as you're giving.
Dr. Gregory Sanders (38:27.138)
And walked into the room. Yeah, I walk into the room and remember guys in a blue gown IV. I start talking to him. He starts asking me about hockey. I grew up in Canada. I'm going to stick. I'm going to stick around and talk about hockey. His phone rings. He says it's your office. I said, it. Hangs up the phone. says, well, that was your office saying we know you're leaving the hospital today. Here's your follow up appointment. Here's your test for your echo. And here's this. And he looked me in the eye and was like, how is this even possible?
Right, so I went from being the disorganized practice that doesn't have anything together to rock star Staff are they happy they're thrilled. They don't have to field phone calls from frustrated people. They proactively call The bottom line is the patient got better care, right? This patient's not going to be lost to follow-up That's an expensive problem very way this patient's not going to be at readmitted because everything's all organized before they even leave the hospital
Yes.
Kaled Alhanafi (39:11.182)
Thank
Dr. Gregory Sanders (39:26.518)
Happy patient, happy staff, better, better top line revenue because you're not bleeding. Win, win, win, win. Yep. OK, so those are the four things. Census management, charge capture, secure messaging, discharge management.
The Win Win
Kaled Alhanafi (39:38.933)
Now the real reason.
So now comes the real reason why I built this. The real reason why I built this is I needed the doctors to have the tool in their hand using it. And then I needed the ability for Hybridchart to monitor and observe the doctor's behavior and do all the things we want to do for value-based care and for population health management, but do it automatically without bothering the doctor. Correct. So if you ask the doctor to be your primary entry point, background.
Dr. Gregory Sanders (40:09.954)
to drive value-based care. And if this is a high-risk heart failure patient, doctor, you need to push this button. Big problem. Number one, the doctor's not gonna do it very often. Because they're busy. Number two, when they do get around to doing it, they're gonna do it too late. Problem. So how does the system say, hey, the doctor just saw a patient put in an ICD-10 code that's in the heart failure family, they're in the ICU.
And that was a high level CPT code. Wait a second. I think this is a high risk heart failure patient. And then automatically, doctor doesn't do anything. All they did was go to the ICU and see a patient put in their charge in two seconds. Automatically, hybrid chart, secure messages, the heart failure nurse saying, we got a live one. Automatically enrolls them in the heart failure clinic. Automatically sets up transitional care medicine. Automatically sets up telemedicine visit or a nurse visit or a home visit. the main
Dr. Gregory Sanders (41:03.606)
Automatically orders them a BNP level and an echo cardiac like but the doctor didn't do anything Okay, so I can hardwire that But the value of building hybrid chart was giving the customer the ability to build their own data model and then develop the rules of engagement Okay, so that whole path we call the pathways that pathway I just described to you. I saw heart failure patient all this stuff happened. That's not hard coded. That's soft coded, right? So the
Yes.
Dr. Gregory Sanders (41:33.294)
practice says, here's what I want to measure. Here's the behaviors I care about. And here's what I want to happen afterwards. And when I put this tool into the hands of an orthopedic surgeon, I have no idea what they care about. So I had to build the model for them to be able to build their own version of my heart failure patient. Because I don't know what it is. And it changes all the time. But none of this is possible if you don't give the doctors a tool that they will actually use.
That's amazing. That's incredible.
Dr. Gregory Sanders (42:02.156)
Otherwise, great idea, never gonna happen.
You have to give them something they love using and they see value in in order for you to do all this work on the back end and capture that pathway.
So you have to figure out what is their pain point because as much as doctors want to help the whole ecosystem, they are too hyper-focused on their own pain in their own world to care about the whole ecosystem. It's not a dig on doctors really. mean, because they're caring people, they're taking care of humans, they're compassionate people. They just don't have the bandwidth. They just simply don't.
always busy. I see my friends, our customers, working until 3 in the morning, charting, doing all these things. It's not easy.
Correct. So the trick was get it in the doctor's hands. The only way you're gonna do that is if you really figure out their pain points and if you really give them a tool that they go, this is great. Okay, that's step one. Step two is build a system where all the VBC population health stuff can pour out of the system automatically. And then I think step three and four is what are the recipes that we need to use to make this happen?
Dr. Gregory Sanders (43:14.668)
What are the executes, like how does all this stuff get executed down the line? It's one thing to say we have a high risk heart failure patient, how does all the stuff actually happen? That's a challenge too.
get done. That's incredible. I think this is something that all of the practices that we're working with would be interested in. And I think a lot of them do know about hybrid chart, which is great. And we have a couple of common partners that we work with. Tell me about what we can do potentially together. So I know you know about our solution and the automating the faxes and the phone calls within the practices. You're figuring out this really
a neat piece around the hospital rounding, having everything happen automatically so that it gets to the practices. Where do you see an opportunity for synergy here? Beyond, of course, we know a lot of people that would be interested in your stuff. You know a lot of people that would be interested in our stuff. From a product perspective, how could that be interesting?
Well, let me start by first saying that you've done a good job solving your space. So I think it's a very, very labor intensive process right now. It's got the same themes that I was trying to solve in my space, which is there's a lot of paper, there's a lot of clunky processes, a lot of human resources go into solving problems that is unnecessary. And then there's delays and the delays impact patient care.
So I think you're probably solving the same types of problems we are just in a completely different space. And I think your product is doing a good job of that. I think that we are a natural feeder into your product, not for all patients, because in your world, if I'm a primary care doctor and I want to send a referral to my office for a cardiology consult, that has nothing to do with hybrid chart. And you solve that problem all day.
Dr. Gregory Sanders (45:10.636)
It's more of, hey, I got a patient in the hospital. I just gave you a whole story about a patient who's leaving who needs care. Well, that's the execution part. So instead of somebody seeing on the hybrid chart dashboard who's coming out of the hospital today and they need an appointment, what if we could eliminate that step? That's the execution step. What if we could feed you the patient saying, here's the guy and they need an appointment and you take care of it? And you engage with the patient, you engage with the practice.
and you take care of it, that's one less potential loose end where something's gonna fall through the cracks. And so, I think that's probably the natural progression of how we can be a natural feeder for you to seamlessly button that up. And I think that just makes more bandwidth for everyone. So let me just sort of talk a little bit about a practice administrator.
Yes, please.
these poor practice administrators. First of all, their job is impossible. Say it out loud. Their job is impossible. They have everybody upset with them. They are wrangling RCM, human resources, a bunch of doctors who won't listen to anything. And everybody's out of bandwidth. And then if you look at all the solutions out there, they're always saying, how can I make the doctor's life better? How can I make the RCM's life better? And then
Very hard job.
Dr. Gregory Sanders (46:34.816)
Is there anything that says, how can I make the practice administration life better? No, there is nothing out there. the way well, well, sort of indirectly your product, too. So how do you help the practice administrator? Well, what you do is you solve the doctor's problems, solve the RCM problems, you solve the schedulers problems, right? You solve your data mining problems. And now the practice administrator actually has the bandwidth to do what they should be doing.
Until now.
Dr. Gregory Sanders (47:01.208)
which is kind of being the CEO of that practice and running it instead of putting out garbage everywhere and having processes that they have no visibility in that are clunky, that are. Fires every day.
Kaled Alhanafi (47:12.3)
turn, the annual work, yeah.
and your staff are burning out, your doctors are burning out. I mean, it's just an impossible thing. So I think our products can help practice administrators by getting off their plate stuff that really doesn't need to be there in the first place.
Love it. Very excited about it. Let's continue that conversation as well. I want to end with a kind of a personal question. In my research, I read that you are the cardiologist or you were the cardiologist for the Suns. And then I learned there's a bunch of sport interests there as well. So tell me more about that.
Well, yeah, the sons were a smaller piece of it. So I was the cardiologist for the Arizona Coyotes hockey team for 20 years by accident. I never graduated fellowship and said, I can't wait to be a sports cardiologist. So it kind of fell in my lap in a weird way. I'd only been in Arizona working for two weeks when I was invited to tag along with the actual cardiologist of the Coyotes.
Last name was Valdez and Ruben Valdez and he looked at me at the, so I grew up in Canada. So he didn't care about hockey at all. And meanwhile, I was like sobbing into a towel through the entire thing. And so at the end of it, he looked at me he's like, you kind of really like this stuff. Do you want to just be the doctor? And I mean, I was like, Ruben, you're trying to hurt me, right? You're kidding, right? So he walked over to the.
Dr. Gregory Sanders (48:42.062)
to the lead doctor and he said, all right, this is your new cardiologist for next year and blah, blah, and you'll meet with him offline. And I called my dad on the way home. like, you're not gonna believe what just happened. So I learned a lot from the Coyotes and from that team and from Bob Liberto, he was the team doc for many, many, many years and worked well with him and his team.
And that kind of spring boarded into working for the Mariners for five years. I did division one ASU for several years for all of their sports teams. There were some Diamondbacks and Suns mixed into there sort of collectively at St. Joe's Hospital. And then I got weird calls during COVID. So I got calls from the San Jose Sharks and the San Francisco 49ers saying, hey, we got kicked out of California.
Half the team has COVID, we need some help. We know you're the doc for the coyotes, like help us out. And so, so I pinch it for them. It's fun.
That's amazing. It is fun and no sleep is right. mean with all of this, being a cardiologist, building a company, selling the product, building it right, coding it, I mean you are a busy man and all doctors are busy but this is on another level. So thank you for making the time. Let me call out.
The the real heroes please as I told you I need a team. Yes, and I need a team Yes, but I didn't mention my real team. Yes, my wife my five kids Like they support me beyond belief. I have the most understanding wife on the planet That's so supportive so enthusiastic Even for today's meeting I was on a bunch of meetings and she walked in she's like you're gonna be late. You cannot be late like what Kristen she was like
Kaled Alhanafi (50:03.63)
team.
Kaled Alhanafi (50:26.402)
What's her name? Thank you, Kristen. Yes.
You gotta go. And I was like, all right, everybody, gotta go. I gotta get dressed, gotta go. So you need a team at home. You need supportive people in your life. I have five wonderful kids who all actively support everything I'm doing. And so I think that's what you need in every area if you want to be successful.
That's amazing. I love that. We should end with that. I'm also grounded by my family and they're the support and for me. so thank you to my wife, Lena, as well and the family. Thank you for being here with us, Dr. Greg Sanders. Really appreciate it. Appreciate having you. Looking forward to more conversations. Thank you for tuning in to today's episode of the Innovators Podcast. I'm your host, co-founder, CEO of Basada Khalid al-Hanafi. Please like, subscribe and share. Thank you. See you next time.
Thank you, Lena.
Ready for your administrative breakthrough?
Get in touch today and learn how Basata can give your admin team superpowers.